POP at 36 / Story at 50
Almost a year and a half ago, things turned to custard in my life. My son needed major orthopaedic surgery and my beloved dad died of a heart attack. I was devastated. It felt like my world imploded. I was incredibly worried about my son and at the same time grieving hugely for my dad. Added to this – covid complications.
A few weeks later I was at a yoga class, doing a deep squat. I felt a sudden, painful drop inside me – a completely unfamiliar type of pain. Over the next few days it got worse – radiating through the lower part of my abdomen, around into my back and down one leg. Sitting was excruciating and it seemed like there was an egg in my vagina.
I had a sense it was related to pelvic organ prolapse. I’d been told I had a bladder prolapse when I had my son thirteen years before, but apart from occasional incidents of stress incontinence it didn’t bother me. I assumed this was a normal consequence of having a baby. A gynaecologist had told me that I’d need surgery at some stage, but I never thought to ask how I would know when. I had worked in a rest home as a caregiver in the past and had looked after women with prolapses. I thought of prolapse as an old lady’s problem.
Now I know it can happen to any woman at any time. Young, old or anywhere in between; pregnancy or no pregnancy. We’re kept in the dark about this, which is so unhelpful.
I have multiple prolapses (uterine, bladder and rectal). Most likely also levator avulsion on one side, from my son’s complicated delivery. I also have pudendal neuralgia – chronic pain from the pudendal nerve in my pelvis, and I know from an MRI that a 2cm section of the nerve on one side is inflamed. It’s useful to know there’s an observable thing causing the pain, and I try to imagine it shrinking and easing. The neuralgia causes me so much more difficulty than the prolapses.
Since this all started I’ve seen two general practitioners, six gynaecologists/urogynaecologists, one pain specialist, five pelvic physios and one regular physio, one sports medicine doctor, an acupuncturist, a massage therapist, a hypopressives trainer, a clinical psychologist and a psychiatrist. That’s 21 health practitioners. I am single-handedly keeping New Zealand’s professional health economy in full swing. Because of me, they can all buy the latest model Teslas.
Early on in this palaver, I met a friend and was telling her about all that was going on – my dad, my son, me. As she listened, tears were streaming down my face, strangers on either side of us were pretending not to notice. She said “I hope you don’t mind me using this word but this is an ABSOLUTE CLUSTERF**K”. I laughed and cried at the same time. I couldn’t have put it better. That’s how I refer to this time now. The clusterf**k.
I’ve had ultrasounds, bladder tests, two MRIs (back and pelvis), and a huge infuriating battle with ACC (who took more than a year to make a decision on my claim and then declined it). I’ve had enormous amounts of pelvic physio – doing kegels, not doing kegels, learning to relax the pelvic floor, learning how to toilet (who knew that even at 50 years of age, there was more to this than I thought?!), core strengthening, pilates, exercise modifications. Looked at my diet, cut down on alcohol. Trialed various medications for pain. Basically anything and everything – I’ve done it.
I’ve tried at least seven different pessaries that I had to buy, as well as many many more from fitting kits. I’ve tried sea sponges and tampons for support. Now I use nothing, as none of the pessaries fit me properly and they all fall down (possibly because of the avulsion) and irritate the pudendal nerve, making the sitting pain even worse. I feel like spray-painting all the pessaries with glitter and turning them into a mobile to hang somewhere – what an enormous waste of money they’ve been for me. The shapes are so interesting – rings, donuts, cubes, and the probe for the electrical stim was like a baby’s dummy. It’s like my body became an adult version of a toddler’s shape-sorting toy.
I’ve felt heard, understood and well-supported by some health professionals (my GP and the pain specialist have been the best) and I consider the treatment I’ve had by some others to be substandard. On one occasion it was so bad I would consider it medical trauma. Another time, a locum GP told me I didn’t have prolapse at all. She thought it was a bladder infection. I said, “you’ve got to be kidding – I can feel it, my wife can feel it.” Clearly she needs glasses (or some training, urgently).
Most specialists have advised me not to have surgery because I already have chronic pain, and surgery can sometimes cause that (in people who don’t have it) or make it worse. I’m ok with no surgery at the moment because I’m concerned about how it often has a shelf life and needs to be repeated. And it can have a lot of complications. It is life changing for some people, and that’s great. I’m scared it might make things worse for me and I don’t know how I would cope with that. This is hard enough as it is.
I would really like a lot more research to happen, so that people with prolapse have more successful treatment options – both pessaries and surgery. Why can’t someone 3D-print a pessary that actually fits each body? If these problems happened to men, there would be many, much better treatments available. This makes me furious.
One specialist said he could offer me surgery, but it would have to be done “very carefully”. So how does he usually operate – carelessly, with his non-dominant hand, while playing Minecraft and sloshing down a Heineken? (I did a PhD in medical communication and honestly, some people could do MUCH better.)
I’ve had two injections of anaesthetic into the pudendal nerve for the pain, and a steroid injection on one occasion too; they gave me immediate relief from the pain, but unfortunately it was temporary. I’ve had electrical stimulation, internal myofascial release, amitriptyline cream, and I take pregabalin and venlafaxine. I’ve had EMDR for birth trauma (very useful). I do hypopressive exercises most days (also useful – my posture is better, my core is stronger, I sleep better and a lot of other aches and pains have disappeared). I do floor-based core and glute exercises; I don’t sit and watch TV, I lie on my yoga mat and do my exercises. This is perfectly normal to my son and wife, but awkward if visitors come round. Some of the exercises are quite unflattering manoeuvres.
I have one option to solve the pain. I could have nerve ablation – where they remove the inflamed part of the nerve. This would leave me with a permanently numb vulva. What kind of a half-arsed (!) choice is that? I can keep pleasure if I put up with pain, or I give up both. Honestly, medicine – you need to UP your game.
I’ve learnt to use meditation and writing to help me manage all this, and one of the best things for me is to get on stage and perform stand-up comedy. That’s amazingly motivating and therapeutic – and I get to laugh with the other comedians, who are like another family for me. I also have some very good, kind, compassionate friends who have let me vent and cry on their shoulders and rage against it all, as much as I’ve needed to. I’m immensely grateful for them. I’ve become much, much better at talking about this stuff and we’ve had some very funny conversations about it all.
My wife has been incredibly patient, caring and loving with me through all of this, even though she can’t always relate to what I’m experiencing. She’s had to take on a lot more at home – I struggle with cooking at the end of the day if the pain is bad, and bending down to garden is out of the question.
My son once said, “I’m sorry that me being such a big baby left you with all this pain”, and I felt terrible. I’ve never said that to him. I replied that I think a whole lot of things contributed, not just his birth. I’d hate him to blame himself. But I’ve found it hard to consolidate my huge love for him with the fact that a traumatic birth was one of the contributors to this.
Overall, this has been incredibly hard. I’ve always been a fit and active person – doing some kind of exercise or physical activity every day. Maybe I did too much. I know now that my body gave me signals, when I rehearsed for dance performances, that my pelvis wasn’t happy. I didn’t know what those symptoms meant.
I’ve had to give up so many things I loved: dancing (afro fusion and hip hop), running, cycling, tennis, skiing. Right now anything high-impact is out. I don’t do much yoga (except trauma-sensitive yoga, where I can choose how I move) as it scares me because that’s where things kicked off – even though I know that’s irrational and most likely it won’t happen again. But how can I be sure? I don’t trust my body the same now, and I’m not sure how to regain that trust.
My work days are difficult as I’m a clinical psychologist and spend a lot of time sitting, listening and attending to other people’s pain – while experiencing an enormous amount myself that my clients have no idea of. I’ve changed my whole work life so that I have more control. I now work for myself and modify my days according to how I am. I spend a lot of time lying down, and a lot of time standing – and as little time sitting as possible.
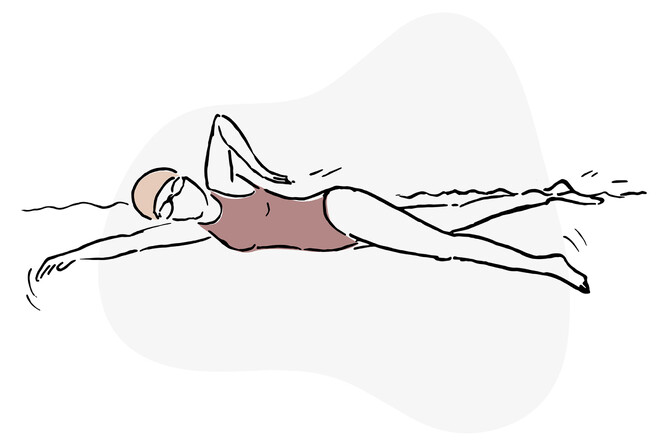
Over time, I’ve found ways of moving that work for me. I walk more and it’s therapeutic to get out in nature. I’ve come to love swimming and I’m much better at that than I used to be. I use flippers as that makes it easier on my pelvis, and I don’t do breaststroke legs as that way of kicking reliably makes the pain flare up. I do mat and reformer pilates, which has been pivotal to bringing me back into my body and moving in ways that feel safe – a good level of challenging. Over the summer I managed some backyard badminton with my family and it was fine, so maybe I’ll get back to tennis one day. I dance a little bit at home and I might try solo salsa classes again at some stage – there’s more controlled movement there, so that might work for me.
I know things that help when the pain flares up. The best thing is a long Epsom salt bath, which I assume makes the pelvic floor relax. If it’s not a bad flare, that works. I also use techniques from Alan Gordon’s book ‘The Way Out’, which has been a game-changer for me.
Despite all this I hit rock bottom in December last year. I couldn’t see a clear pathway forward. My symptoms were still basically the same. I could imagine my son and wife off enjoying bike rides together and I wouldn’t be able to go, unless I was ready to potentially have days or weeks of pelvic agony afterwards.
I’d been having bleak thoughts for a while and was having them again. It wasn’t that I didn’t want to live, but I didn’t want to go on in THIS BODY, with no reprieve in sight. My wife and I talked for what seemed like hours and the next day I decided to start taking the venlafaxine (an antidepressant), which the pain specialist had prescribed weeks before. It helped pretty much from day one, even a low dose. I still have enormous amounts of pain sometimes but it doesn’t get me down as much.
Then another pivotal thing happened. I talked to pelvic physio number five by telehealth – a woman who has prolapse herself and has managed it for decades. She also knows a huge amount about pelvic pain. She said a number of things that were helpful. One is that the pelvic floor is our body’s first responder – it tightens all the time when we hear or experience anything difficult. Since she pointed that out, I’ve noticed it’s true. She also told me about the ‘sit like a man’ philosophy. As women, we inadvertently pressure our pelvic floors by crossing our legs, holding our knees together and generally keeping ourselves small in the ways society has taught us to. Since then I’ve been womanspreading whenever I can and it’s great. We need to start a worldwide movement.
The biggest turning point for me, though, was when she said, “I’m hearing the narrative of a broken woman”. She was 100% on the money. That’s exactly how I’d been feeling since this started. Broken, defective, faulty, impossible to fix. As soon as she said it, I decided not to think of myself that way any more. Not in a toxic positivity way – I can’t pretend none of this is happening and I’m not going to be looking for the silver lining and posting #blessed about it all over social media.
But here’s how I’m approaching it now: I'm not broken. This isn't going to define me. It's a big thing and brings many challenges but I'm not letting it control my life to the extent that it did before.
Realising this has been utterly liberating. When the pain comes on, I notice it but don’t give it much airtime in my mind. I don’t talk about it much. I know it will come and go, and I still need to manage it. But it doesn’t get to control my life.
I’m so much more than my pelvic issues. And if you have challenges with this part of your body – so are you.